FlexBand
Inflammation in Acute Ankle Sprains
The role of inflammation in acute injuries is to enhance the flow of blood cells and chemical mediators to the site of injury. Upon arrival of these cells and mediators at the site of injury, they destroy, dilute or wall off all injurious agents and allow repairing cascades to being.
There are several distinct phases of the inflammatory process, each serving a unique purpose towards repair and healing. The initial stage results in reduced blood flow through the small arteries (arterioles) by means of vasoconstriction. This typically lasts 3-5 seconds. If you have ever cut yourself, you know that initially there is little bleeding at the site of injury. Arteriolar vasoconstriction is the reason why this happens.
This is quickly followed by vasodilation of these same arterioles as well as opening of the small vessels in the neighboring capillary bed. Heat and redness are the cardinal signs of this phase. As these vessels engorge with blood, the hydrostatic pressure raises, which leads to leakage of plasma and plasma proteins out of blood vessels and into surrounding tissues. The result is localized swelling. Removal of these fluids and the swelling they cause happens via thin draining channels called the lymphatic vessels. This is a passive process that occurs slowly and is aided by both muscle contraction and elevation.
Ankle Rehab Kits
2-5-2014
"I am excited about what I learned from Doc Shimmel's treatment with compression bands & flexband traction for ankle sprains. Looking forward to spring training to show the rest of the staff what I learned"
Matt Johnson
Assistant Athletic Trainer
Chicago Cubs
This patient was able to return to full sports participation in less than 2 weeks!
AKRON, Ohio - Sophomore Rob Brandenberg rolled his left ankle in practice Wednesday, and his status, although not publicly released, was up in the air prior to Thursday's 76-75 win at Akron. It was an importnat game for both Brandenberg and VCU. The Rams' shooting guard is from Gahanna, Ohio, about two hours from Akron, and a large contingent of friends and family would be in attendance. Meanwhile, VCU was playing a tough road game in a packed arena. If Brandenberg couldn't play or would be severely restricted, it would be a significant setback for the Rams.
Although he did not start, Brandenberg played 23 critical minutes and provided several key buckets to spark the VCU win. He finished with 11 points and hit 4-of-6 shots from the field. A 6-foot-3 guard, Brandenburg could be seen wincing on occasion, but his play did not look like that of a guy with a bum wheel.
It turns out there was a good reason for that.
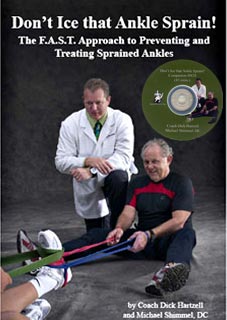
VCU's strength and training staffs have, of late, subscribed to the treatments of Dick Hartzell and Dr. Michael Shimmel, who co-authored "Don't Ice That Ankle Sprain!". Hartzell and Shimmel write, in part, that icing an ankle actually impedes the healing process. Instead, they use a series of stretches and range of motion exercises with an elastic stretch band, which they claim greatly reduces recovery time. When Darius Theus rolled an ankle earlier this season, the Rams' training staff used those methods at halftime to get Theus back in the game.
Hartzell is a Youngstown, Ohio native, while Shimmel resides in Stow, just miles from the University of Akron campus. VCU Strength and Conditioning Coach Daniel Roose remembered that the duo were Northeast Ohio natives and managed to contact Shimmel Wednesday night via e-mail. Shimmel volunteered to come to VCU's hotel Thursday to run Brandenberg through an hour's worth of treatments prior to the Rams' game. The rest is history.
Related Videos
With the leakage of plasma proteins and fluids out of the vascular bed, the blood becomes more viscous due to relative increasing concentrations of both red and white blood cells remaining inside the blood vessels. This increases viscosity, which serves to slow blood flow enough to allow white blood cells responsible for tissue repair to move more slowly towards the vessel wall where they attach temporarily. After they adhere to the inner walls of the blood vessels in a process called margination, they are able to migrate through the vessel wall and into surrounding injured tissues.
The arrival of white blood cell lines in the surrounding tissues results in the release of digestive enzymes and an entire cast of chemical mediators from "activated" white blood cells that aid in tissue "clean-up" and repair.
Unfortunately, sometimes these chemical mediators can cause additional destruction of healthy tissue or excessive scar formation by cells called fibroblasts, particularly when inflammation persists.
With this background on the purpose and process of inflammation in injured muscles, tendons, and ligaments, let's consider modes of intervention which could prevent further tissue damage and accelerate repair. This standard RICE approach contains aspects of merit, but also significant flaws which may be counterproductive.
Rest ("R") is the standard approach for sprains. The principle behind it is that pain serves the purpose of warning us against continued activity which could further extend the injury. While no one would consider sprinting all-out immediately after a bad ankle sprain, prolonged rest is likewise harmful.
Rest results in muscle, tendon and ligament atrophy (shrinkage) which then leads to further weakness and re-injury. Rest also results in dampening of signals from nearby sensory nerve fibers which normally serve to assist with balance and proper body positioning. Therefore, the absolute worst intervention in complete rest! Generally, the sooner one can get the joint moving through its normal range of motion, the less likely surrounding connective tissues and nerves will be to lose their intended functions.
Observations in the medical world also bear out this point. It is standard protocol now following open-heart surgery to encourage walking within 24 hours of surgery by adequately treating post-operative pain. Many open-heart patients have been known to go home only four to five days after surgery, primarily due to the speed of recovery that early activity promotes! On the contrary, individuals who are made comatose by artificial or chemical means for any extended period of time experience a tremendous loss of lean body mass and have a very prolonged recovery once they are allowed to "wake-up". Often, severe infections and a multiplicity of other organ system complications develop while a person is at complete "rest". In short, rest leads to atrophy and weakness, while movement enhances healing and vitality because it stimulates blood flow.
Ice ("I") is the next step in the long-standing treatment for any sprain, bruise or soft tissue injury. Most circles endorse ice for the first 48 hours following soft tissue injuries such as sprains. This practice should be seriously challenged. The theory has been that ice restricts blood flow and reduces swelling, thereby minimizing pain. As outlined above, the inflammatory process is well orchestrated, each step both serving a purpose and acting as a precursor for the next. Leakage of blood plasma into surrounding tissue with subsequent swelling allows for the healing and repairing blood cells to find their way to the site of injury. If ice is truly able to restrict blood flow, how would these repairing white blood cells find their way to the site of injury?
The application of ice penetrates only a few millimeters of tissue and therefore may not be operative in deeper tissues. Furthermore, the highly complex clotting system is a quick-acting system that stops most active bleeding by the time ice can be applied. Finally, ice usually results in inactivity, at least during the standard 15-20 minutes of application. Valuable time may be sacrificed during icing that could be put to better use trying to enhance joint re-alignment and mobility.
Compression ("C") is the third principle in the RICE method and, like ice, is directed towards reducing swelling. This step makes some sense, because it attempts to interrupt the inflammatory process by preventing the elevation of arteriolar hydrostatic pressure. While compression may limit some tissue edema, it may also assist in lymphatic drainage by preventing thin lymphatic walls from being compressed by excess tissue edema.
Elevation ("E"), like ice and compression, is the fourth mechanism of limiting tissue swelling. While elevation may limit tissue swelling to a degree, its primary value may be in enhancing lymphatic drainage from the site of injury and edema. In short, the inflammatory process has been designed not as a means of extending injury and prolonging recovery, but as a means of orchestrating tissue repair. Personal experience as a physician has shown me that the RICE approach often delays recovery.
A more logical approach involves restoration of joint alignment with the associative muscles, tendons, ligaments, nerves and blood vessels as quickly as possible after injury. Minimizing swelling can also be an objective to reduce pain without interfering with the inflammatory process. By quickly elevating the injured limb and applying gentle but progressive traction on the joint, normal alignment can be restored before pain sets in and muscle contraction and loss of mobility occur in response to pain. With the limb elevated, compression wraps or preferably gentle massage can be performed to "milk" the edema out of the injured tissue into the draining lymphatic vessels.
The overall goal of early sprain intervention is two-fold: to minimize excessive swelling and to enhance tissue blood flow. Excessive and prolonged swelling should be minimized by appropriate means in order to reduce pain and assist in the return of natural range of motion. Early, gradual, and progressive movement of the injured joint in ranges of motion that do not exacerbate pain enhances recovery. Traction is an especially effective way to encourage movement. It can be accomplished by means of a giant rubberband (Flexband®). With the joint placed in gentle traction, movement in all directions can be initiated in order to help re-align injured ligaments, tendons, muscles, and nerves.
As I mentioned, the second goal of sprain recovery is enhancing tissue blood flow. Blood heals. Surgeons know this. Patients who have impaired blood flow from advanced heart disease or diabetes take loner to heal. A one-inch cut on the face requiring stitches normally requires three to five days of healing before the stitches can be removed. The same cut and repair on the leg requires seven to ten days to heal. Why? The face heals faster because the blood supple is greater.
The recovery process of any sprain is accelerated by blood flow. Movement is the mechanism for enhancing blood flow. The key to recovery is gradual, progressive and relatively pain-free movement in all directions the joint is intended to move. As Coach Hartzell says, "Rest is for the deceased!!!" Order your copy of Don't Ice That Ankle Sprain now.
--- Tim McKnight, MD
*User please seek advice of a medical professional prior to using the product and/or attempting to use workout/rehab information.